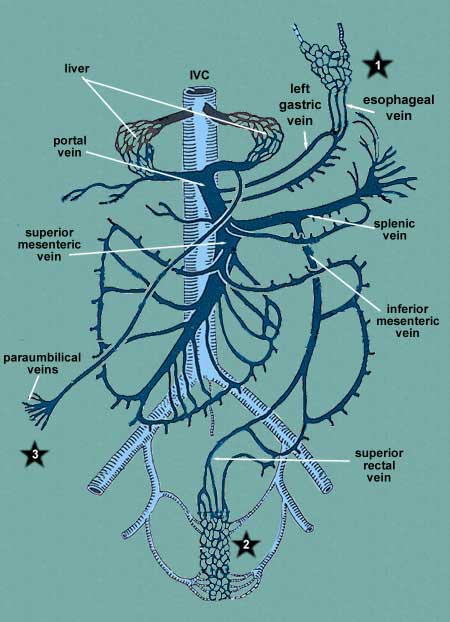
Clinical Consideration
Portal obstruction. In cases of liver disease
where the portal blood can no longer pass through the liver, the blood will
try to get back to the heart any way it can and this usually involves the
superior or inferior venae cavae. One possible cause of liver disease is chronic
alcoholism. When the liver becomes impassable, it will pass backwards through
the portal vein into the left gastric, paraumbilical or superior rectal.
At each of these sites, the veins become enlarged and will result in other
clinical signs and symptoms.
In case of the
esophageal plexus (*1), esophageal
varices will develop and massive hemorrhage may occur resulting in death.
In case of the
rectal plexus (*2), hemorrhoids
occur, resulting in pain and bleeding.
In case of the
paraumbilical veins (*3), visible
signs of venous enlargement and tortuosity occur on the abdomen and these
are referred to the
caput medusae.
Caval blockage. In cases where tumors or other
pathologies compress the vena cava, the blood will utilize the above connections
to return blood to the heart but this time through the caval system.