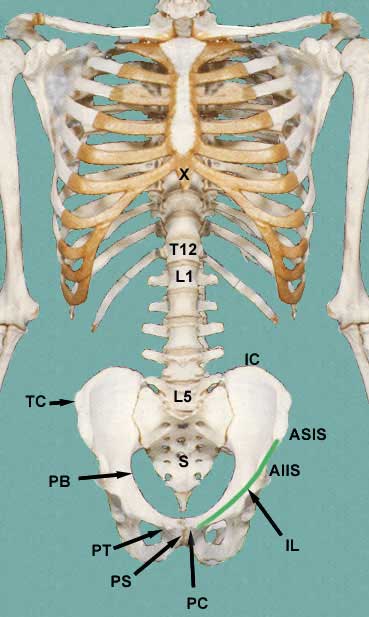
Skeleton of the Abdomen
|
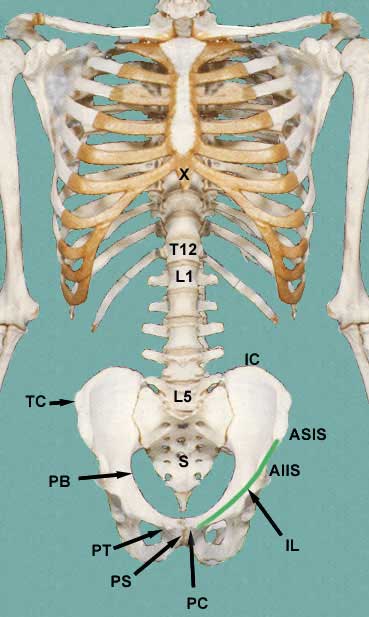
The skeleton of the abdomen is represented in the adjacent figure.
Starting from the from we have:
- xiphoid process X
- costal cartilages (ribs 7-10)
- tips of ribs 11 and 12
- vertebrae L1-L5
- iliac crests IC
- tubercle of the crest TC
- anterior superior iliac spine ASIS
- anterior inferior iliac spine AIIS
- inguinal ligament IL
- pubic tubercle PT
- pubic crest PC
- pubic symphysis PS
- the separation of the abdomen from the pelvis, the pelvic brim
PB
|
|
The inguinal ligament extends from the anterior superior iliac spine ASIS to the pubic tubercle PT and is used as one of the lower
borders of the abdomen. This ligament is really a turned under edge of the
aponeurosis of the external abdominal oblique muscle. We will mention it again
when we cover the inguinal region of the abdomen.
The thoracic diaphragm separates the abdominal cavity from the thoracic
cavity.
Abdominal Wall
Surface Anatomy of the Abdomen
| Before getting into the nitty gritty of the abdomen, keep in mind that
you want to be able to use your knowledge to project the anatomy onto the
surface of the abdomen. You will want to be able to visualize the relative
positions of abdominal organs as they lie within the abdomen. Clinicians
might use several different ways of subdividing the surface of the anterior
abdominal wall but I will only present two of them here. By subdividing the
surface into regions, one person can tell another person exactly where to
look for possible problems.
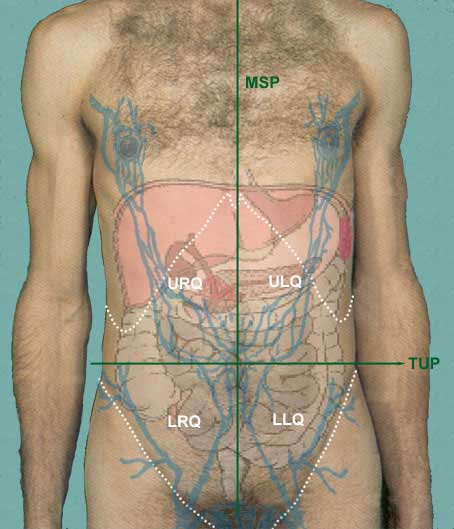
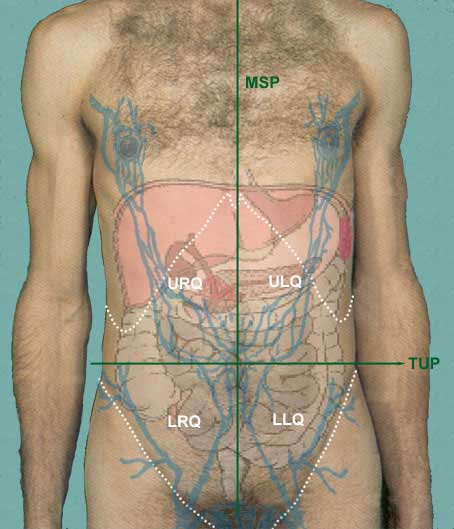
The easiest is to separate the surface into 4 quadrants:
- upper left quadrant ULQ
- lower left quadrant LLQ
- upper right quadrant URQ
- lower right quadrant LRQ
These quadrants are developed by dropping a vertical line down the
middle of the sternum MSP and
a horizontal line across and through the umbilicus TUP
|
|
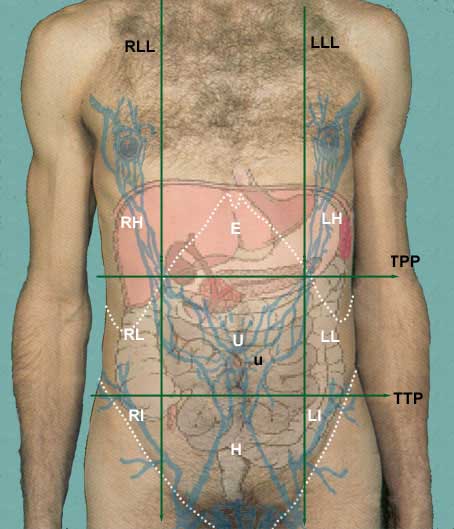
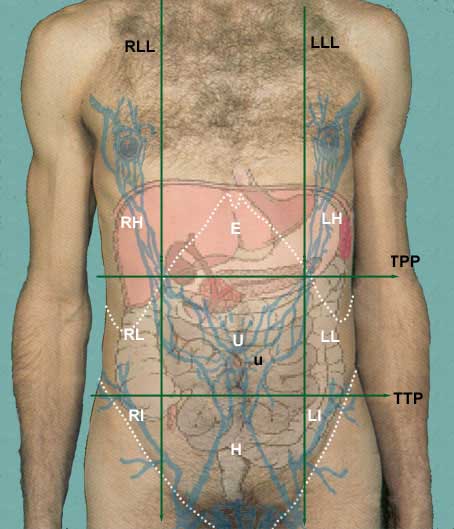
The second way of dividing the abdominal surface is into 9 regions:
- left hypochondriac LH
- left lumbar LL
- left iliac LI
- epigastric E
- umbilical U
- hypogastric H
- right hypochondriac RH
- right lumbar RL
- right iliac RI
These regions are formed by two vertical planes and two horizontal
planes. The two vertical planes are the lateral lines LLL and RLL. These lines are dropped from
a point half way between the jugular notch and the acromion process.
The two horizontal planes are the transpyloric plane TPP and the transtubercular plane
TTP. The tubercles are
the tubercles of the iliac crests.
|
|
As a student of anatomy, it is sometimes fun to pretend that you are going
to be a surgeon and are, at this point, considering entering the abdominal
cavity to remove or reconstruct something in the abdominal cavity. It would
helpful if you knew what makes up the wall of the abdomen so that you would
be able to judge how deep you have gone with each knife cut. This brings
us to the discussion of the abdominal wall.
When considering the abdominal wall, you will need to know where, specifically
it is that you want to enter.
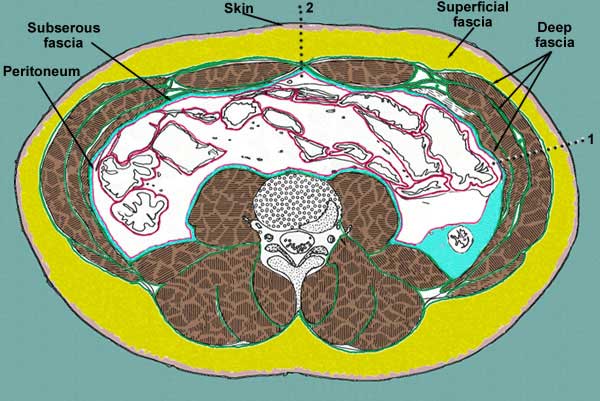
Layers of the Abdominal Wall
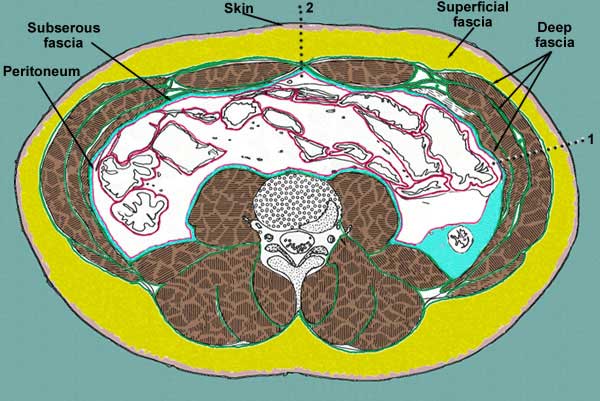
The layers of the abdominal wall vary, depending on where it is you
are looking. For instance, it is somewhat different along the lateral sides
of the abdomen than it is at the anterior side. It is also somewhat different
at its lower regions.
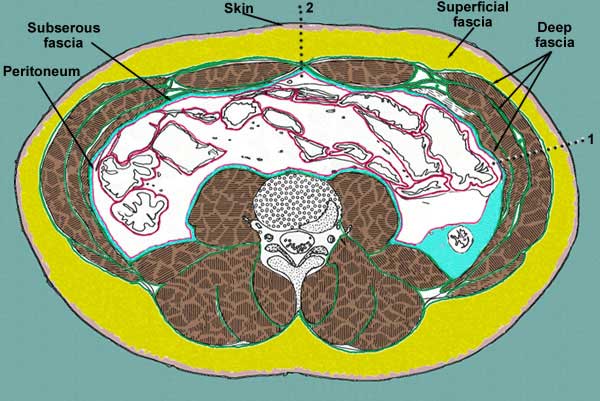
Lets start out along the lateral side of the abdomen:
- skin

- superficial fascia

- deep fascia

- muscle

- subserous fascia

- peritoneum

|
|
At the lateral side of the abdomen (1) there is a dotted line passing
through the abdominal wall. Note the layers a surgeons knife, a criminal
knife or a anatomy student's knife must pass through to get to the peritoneal
cavity:
- skin
- superficial fascia (this may be as thin as or less than a half
inch or as thick as 6 inches or more)
- deep fascia (all skeletal muscle is surrounded within its own
deep fascia). The deep fascia of the abdominal wall is different than that
found around muscles of the extremities, however. It is of the loose connective
tissue variety. It is necessary in the abdominal wall because it offers
more flexibility for a variety of functions of the abdomen. At certain points,
this fascia may become aponeurotic and serve as attachments for the muscle
to bone or to each other, as is the case at the linea alba.
- subserous fascia also known at extraperitoneal fascia (a layer
of loose connective tissue that serves as a glue to hold the peritoneum
to the deep fascia of the abdominal wall or to the outer lining of the GI
tract. It may receive different names depending on its location (i.e. transversalis
fascia when it is deep to that muscle, psoas fascia when it is next to that
muscles, iliac fascia, etc.)
- peritoneum (a thin one cell thick membrane that lines the abdominal
cavity and in certain places reflects inward to form a double layer of peritoneum)
Double layers of peritoneum are called mesenteries, omenta, falciform ligaments,
lienorenal ligament, etc.)
|
|
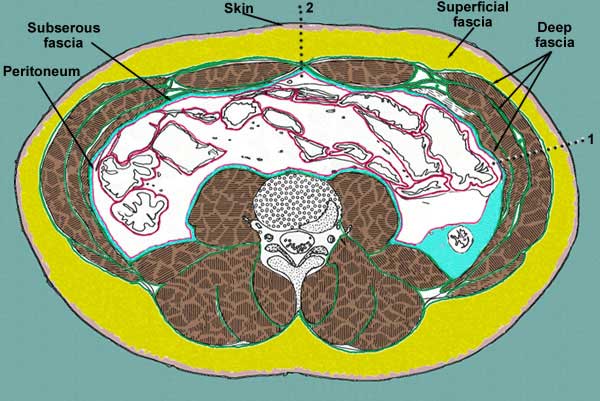
At the anterior wall of the abdomen, in the midline there is no muscle
so a knife would only go through the:
- skin
- superficial fascia
- deep fascia (in this case a thickened area of deep fascia called
the linea alba)
- subserous fascia
- peritoneum
|
|
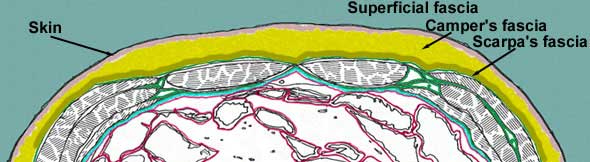
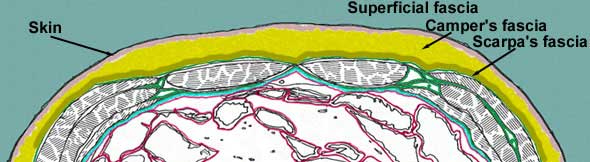
If we look at the wall inferior to the level of the belly button (umbilicus),
you will see that the superficial fascia has become divided into to parts:
- a superficial fatty part that is continuous with the same layer over
the rest of the body (Camper's fascia)
- a deep membranous layer that is continuous down into the perineum
to surround the penis and to form a layer of the scrotum. (Scarpa's fascia)
|
|
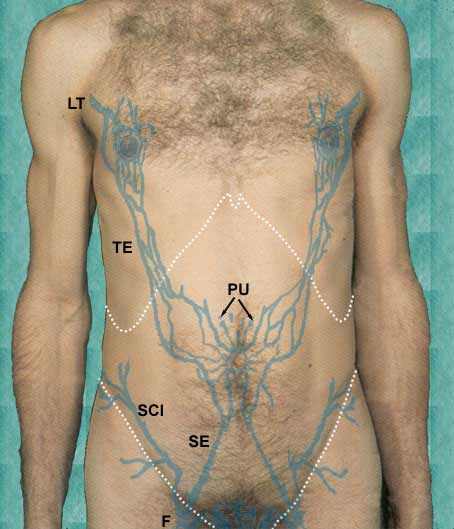
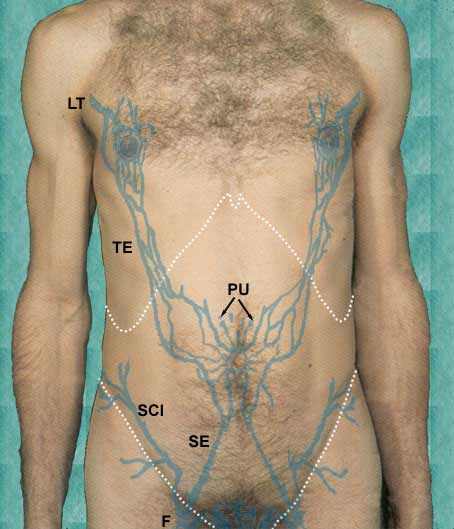
As you examine the abdomen in thin subjects, you may be able to see
the superficial veins that drain the abdominal wall. These veins drain into
one of two major veins:
- subclavian (not shown)
- femoral (F)
and also into a minor, but important vein, the paraumbilical vein PU. The paraumbilical vein drains
into the portal vein and then through the liver. This is an important clinical
connection.
The lower abdominal wall is drained by way of the superficial epigastric
SE and superficial circumflex
iliac SCI veins into the femoral
vein.
The upper abdominal wall is drained by way of the thoracoepigastric
TE and lateral thoracic
LT veins into the subclavian.
|
|
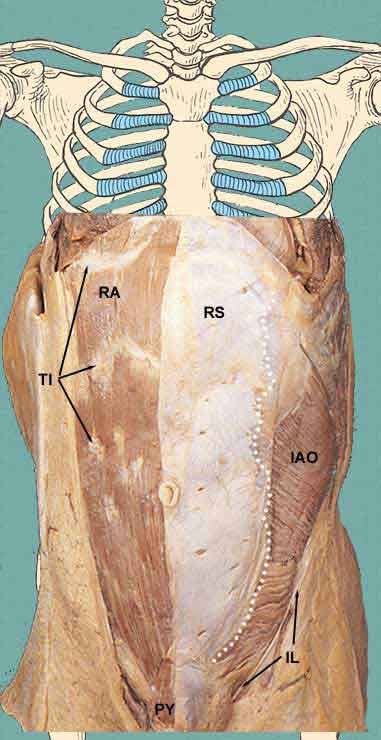
Muscles of the Abdominal Wall
It is now time to consider the muscles that make up the anterior and anterolateral
abdominal wall. There are 4 pairs of muscles to consider. We will remove
layers carefully to see the deeper levels. As we go deeper through the layers,
you should be aware of the cutaneous veins and nerves that travel in the
layers.
The most superficial layer of anterolateral muscles are the:
- external abdominal obliques EAO
Notice on the right side of the specimen that the lower part of the
superficial fascia has been left behind so that you might see its two layers,
the fatty layer (Camper's fascia) CF
and the membranous layer (Scarpa's fascia) SF. Running through the fatty layer
are the superficial veins, the superficial epigastric SE, the paraumbilical veins radiating
out from the umbilicus and the thoracoepigastric vein TE.
The cutaneous nerves to the abdomen are mainly continuations of the
lower intercostal nerves (T7 - T12). An important level to remember is that
the umbilical region is supplied by the 10th intercostal nerve. The lowermost
part of the abdominal wall is supplied by a branch of L1, the iliohypogastric
IH nerve. Its other
branch is the ilioinguinal II
nerve.
You should also identify the linea alba LA. This white line is where the
aponeuroses of the external abdominal oblique, internal abdominal oblique,
and transverse abdominis muscles converge at the midsagittal part of the abdominal
wall.
|

|
|
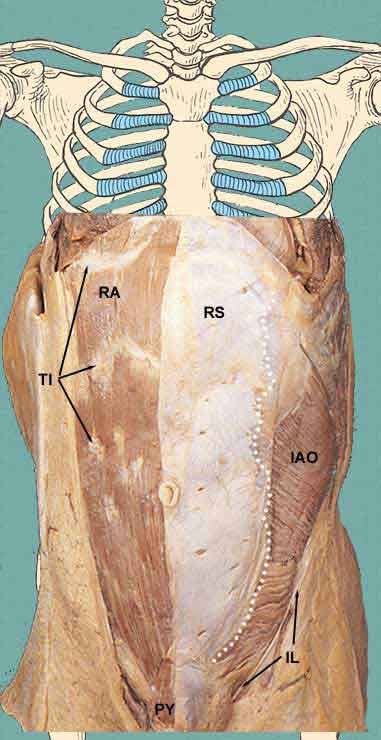
In the image, the left external abdominal oblique has been cut away
at the white dotted line and removed in order to show the internal abdominal
oblique IAO. You can also
see lower cut edge of the external abdominal oblique at the inguinal ligament
IL
The anterior wall of the rectus sheath RS has also been removed on the right
side in order to see the underlying right rectus abdominis RA muscle. Note that the rectus abdominis
muscle is subdivided into small sections by so called tendinous inscriptions
TI. This arrangement is
what forms the wash-board abs in well-exercised people.
We will discuss the formation of the rectus sheath in a moment.
You may also see a small muscle overlying the inferior end of the
rectus abdominis muscle, the pyramidalis muscle PY. This small muscles tenses the
lower part of the linea alba.
|
|
|
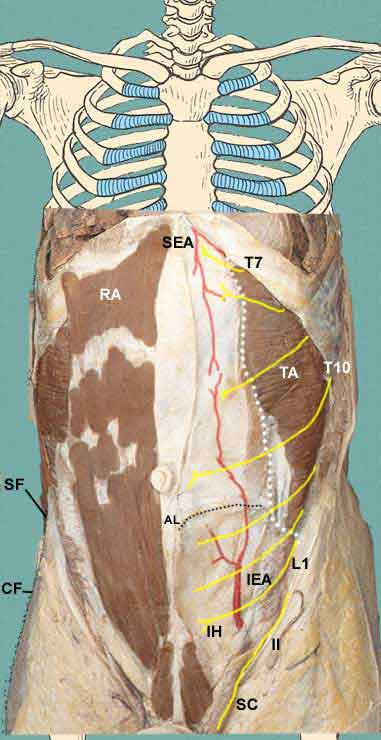
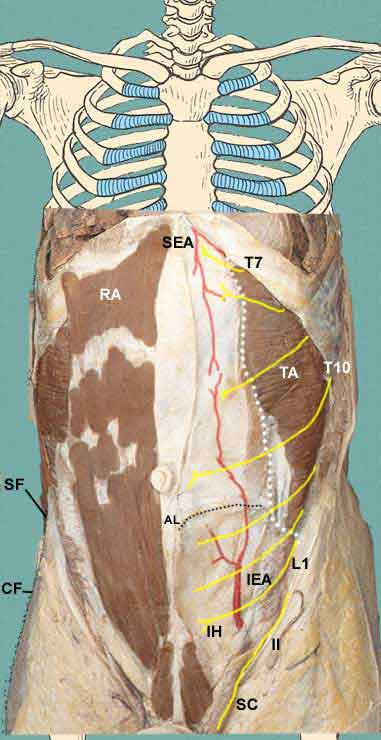
In this specimen, the rectus abdominis muscle, internal abdominal
oblique and anterior rectus sheath have been removed. You can identify the
posterior rectus sheath and its lower free margin, the arcuate line AL. What you see below this line
is the transversalis fascia and running in the fascia is the inferior epigastric
artery IEA, a branch of the
external iliac artery. This artery enters the rectus sheath posterior to the
rectus abdominis muscle and supplies the anterior abdominal wall. Extending
from the top, is a branch of the internal thoracic (or mammary) artery, the
superior epigastric artery.
Also note that the cutaneous nerves are found to lie between the
internal abdominal oblique and the transversus abdominis muscles.
|
|