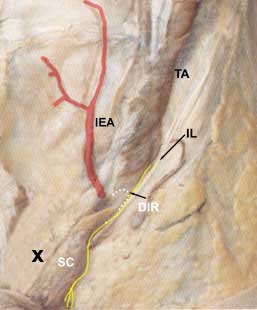
In the second image, the external oblique has been removed and you see the internal abdominal oblique IAO. Notice the cut margin of the external oblique at the inguinal ligament IL. Note that some of the fibers of the internal oblique continue down and around the spermatic cord to become the creamasteric layer of the spermatic cord. These muscle fibers perform an important reflex called the cremasteric reflex, a test performed in most routine physical exams in males.
In the third image, the internal oblique has been removed and you see the transversus abdominis muscle TA. If you look just below the lower fibers of the tranversus abdominis you will see the spermatic cord SC as it passes through the deep inguinal ring DIR. Identify the ilioinguinal nerve as it runs deep to the inguinal ligament. Notice that it does not enter the inguinal canal along with the spermatic cord. The deep inguinal ring is nothing more than a thickening of the transversalis fascia at the point where the structures that make up the spermatic cord converge.
|
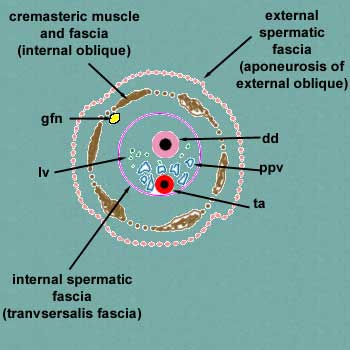
Cremasteric reflex. A reflex is a reaction to some kind of stimulus (stroke, pin prick, etc.). A stimulus is picked up by sensory (afferent) nerves and carried to the spinal cord (central nervous system) where it forms a synapse with motor (efferent) neurons that pass out to a muscle to perform an action. In the case of the cremasteric reflex, the afferent limb of the reflex is by way of the genitofemoral nerve and the efferent limb is by way genitofemoral fibers to the cremasteric muscle. The result is that by stroking the skin on the medial side of the thigh next to the scrotum, the scrotum is pulled up on that side. The spinal cord segments involved are L1 - L2. |